Virginia Tech researchers at the Fralin Biomedical Research Institute at VTC report that applying low-intensity focused ultrasound to an area deep within the brain may point to new ways to help people cope with chronic pain.
In a study published in the Journal of Neuroscience, scientists demonstrated the effectiveness of using low-intensity focused ultrasound to modulate the activity in a critical region in the brain that processes and regulates pain signals.
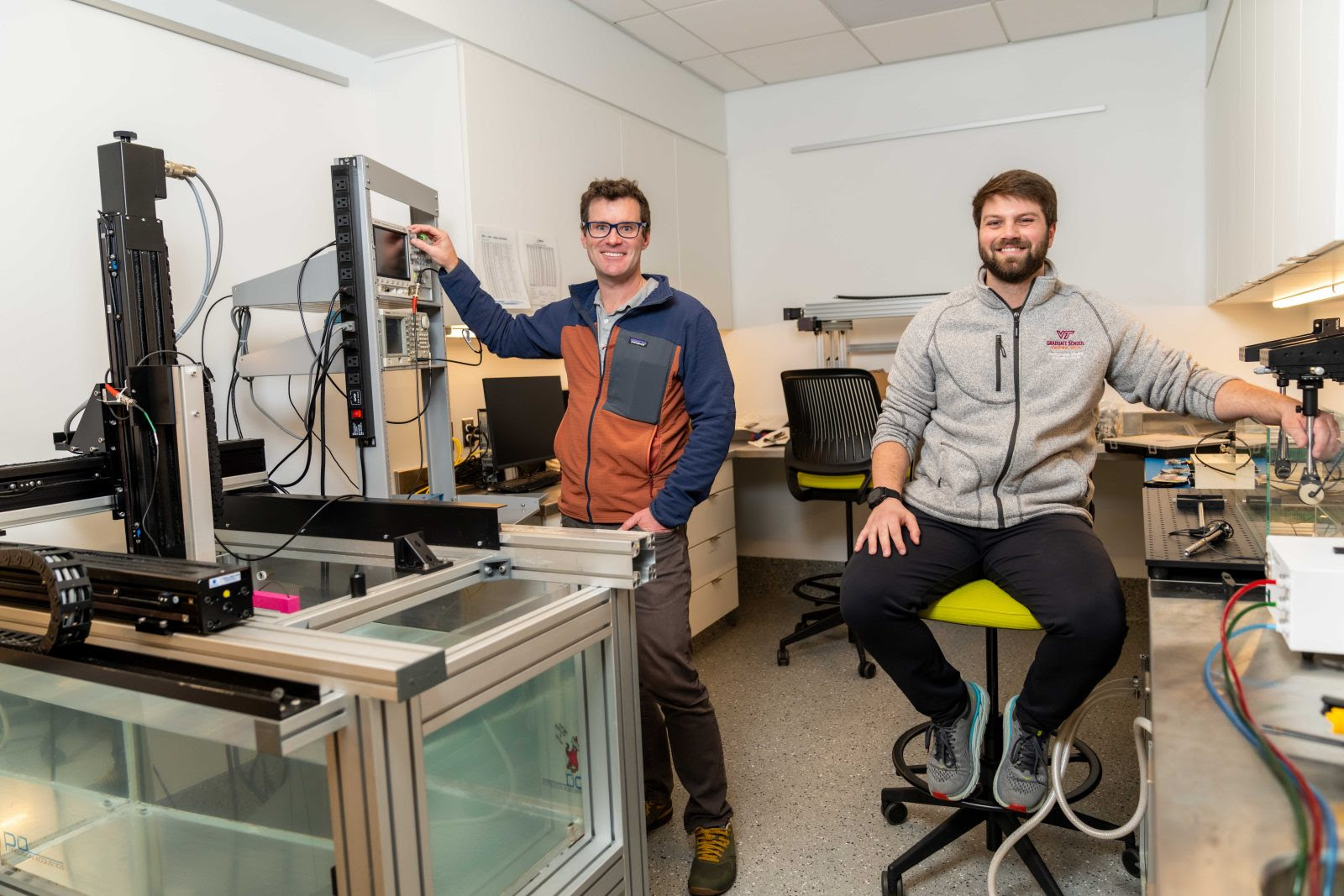
Researchers, including first author Andrew Strohman, a Virginia Tech M.D./Ph.D student conducting research at the Fralin Biomedical Research Institute, found the application of low-intensity ultrasound to a structure known as the dorsal anterior cingulate cortex reduced pain, diminished bodily responses to pain, and decreased pain-related brain activity without the need for invasive procedures, researchers said.
Strohman is a student in the Virginia Tech Carilion School of Medicine and the Translational Biology, Medicine, and Health Graduate Program.
“This study points to a noninvasive and effective way to modulate a critical region of the brain involved in pain processing while eliminating many of the risks associated with surgeries,” said Wynn Legon, assistant professor at the Fralin Biomedical Research Institute and senior author of the study. “It provides a potential new means to modulate the brain activity in response to pain that may serve to better understand the mechanisms of chronic pain to provide a new, innovative therapeutic option that could change how we approach and treat pain in the future.”
In a study with 16 healthy volunteers, researchers focused ultrasound energy on the dorsal anterior cingulate cortex to see if it could change how people feel pain. To test whether it changed someone’s perception of pain, they applied brief heat to the skin and measured pain perception, heart rate variability, skin responses, and brain electrical signals.
Data was collected in three sessions on three separate days along with an imaging visit consisting of a CT scan and MRI to accurately and reliably target this hard-to-reach area in each individual.
The results showed that the ultrasound made people feel less pain, and it also altered how the brain and heart communicate. Overall, the heart did not respond as strongly to pain, and certain brain signals changed.
“Chronic pain patients often experience cardiovascular issues, which may either be at the root of their chronic pain or play a role in contributing to it,” said Legon, who is also assistant professor in the College of Science’s School of Neuroscience and in the Virginia Tech Carilion School of Medicine’s Department of Neurosurgery. “Understanding this intricate relationship is crucial because it enhances our comprehension of pain mechanisms and suggests the importance of addressing both pain perception and cardiovascular health.”
The results suggest that using ultrasound applied to this specific region of the brain may help reduce pain and change how the body reacts to pain.
Even more recently, in a study published in the journal PAIN on Feb. 5, the researchers found soundwaves from low-intensity focused ultrasound aimed at a brain region called the insula can also reduce both the perception of pain and other effects.
“This study provides some of the first evidence we can change three major areas of activity, those being pain perception, brain activity, and cardiac activity,” Strohman said. “The next steps are to look at how these metrics relate to each other and explore how these findings can be applied to improve the lives of patients suffering from chronic pain.”
“While there has been tremendous progress in recent years in the use of high-intensity focused ultrasound for creating small lesions in patients’ brain to treat disorders such as essential tremor and for tumor ablation, we are at the very beginning of exploration of the use of low-intensity focused ultrasound to mildly modulate brain activity and affect perception and behavior,” said Michael Friedlander, executive director of the Fralin Biomedical Research Institute, who was not involved with the study.
“The new work by Strohman and Legon and their pioneering team represents some of the most exciting new advances of this approach,” added Friedlander, who is also Virginia Tech’s vice president for health sciences and technology.
“The fact that it is addressing one of the most debilitating diseases, chronic pain, represents a major step in this important emerging field of biomedical research and provides hope for better treatments that may avoid the untoward effects of many drugs used for treating pain,” Friedlander said.
Research Assistant Brighton Payne, medical student Alexander In, and M.D./Ph.D. student Katelyn Stebbins of the Legon lab at the Fralin Biomedical Research Institute contributed to the study.
The work was partially supported by grants from the Seale Innovation Fund of the Fralin Biomedical Research Institute.
John Pastor for Virginia Tech


